
Even before the pandemic, the healthcare industry was at the inflection point, with continuously rising healthcare costs, growing consumer demand, and evolving care models. COVID-19 has become a catalyst for change, completely transforming the way we access healthcare.
In the face of pandemic-induced challenges and limitations, telehealth served as a lifeline for care providers, helping them deliver the care that patients need while complying with social distancing measures. The Telehealth Adoption Tracker proves the point. In early 2020, telemedicine solutions were used for less than 1% of patient visits. A few months into the crisis, and telehealth usage reached its maximum of more than 51%.
In addition to the increased telehealth adoption, the crisis has created momentum for a number of transformative changes that will define virtual care in the decade to come.
The distinction between online and offline has been blurry even before the pandemic. Consumers buy clothes from an eCommerce retailer and return purchases at the nearest brick-and-mortar store, make a money transfer online and go to the bank to rent a safe deposit box. Now, with the rise of a hybrid workforce and blended learning schools, the hybrid model is becoming an essential part of how businesses navigate the new normal.
Healthcare, too, is embracing the new approach by combining virtual and in-person experiences across the entire care continuum. When the pandemic began, telehealth services were limited to certain use cases like urgent care and telepsychiatry. But what started as a necessity, has quickly become a preferred method of delivering care. As telehealth advantages became more distinctive, healthcare providers started to incorporate virtual care into a wider range of settings.
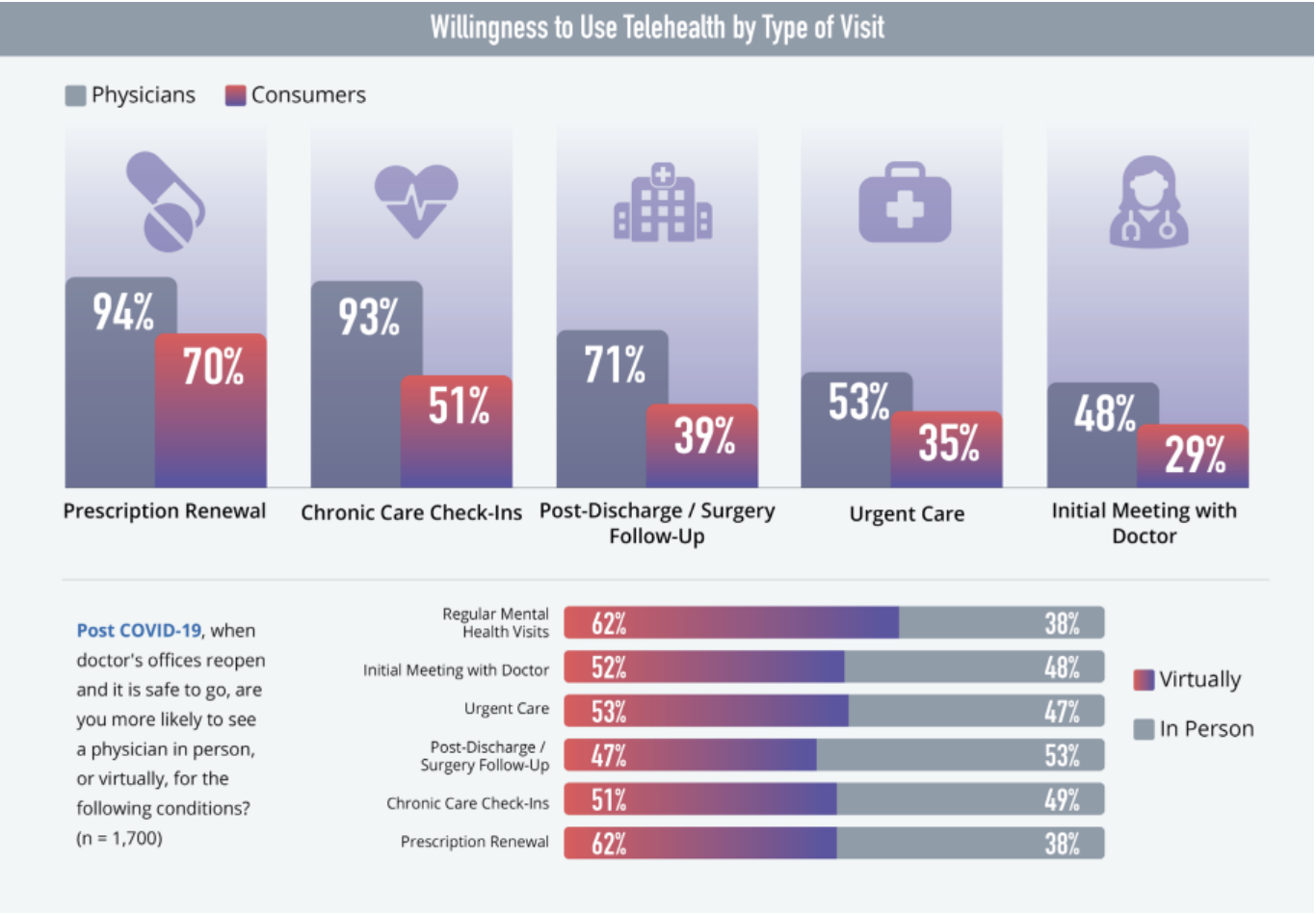
Source: Amwell
Physical, face-to-face encounters like immunizations, labs, procedures still matter and make a significant part of care delivery. But in the post-pandemic world, we’ll see the hybrid model successfully blending in-person elements with virtual care to create a holistic experience for patients and healthcare providers alike.
Telehealth success is pushing innovation in healthcare further and encouraging care providers and consumers to adopt digital health technology on a wider scale. Medical wearables, activity trackers, clinical monitors, smart beds, connected inhalers, and more — the healthcare ecosystem is expanding with the growing amount of digital health tools.
These smart medical devices are able to generate, gather, and analyze vital medical data in real time, enabling remote patient monitoring (RPM) outside of the traditional clinical environment. As the Internet of Medical Things (IoMT) becomes more mature, the next generation of digital health tools will include tech-enabled pills to monitor medication intake, advanced biosensors that track a patient’s exposure to UV radiation, air pollution, humidity, and the like.
The IoMT market continues to grow and is expected to reach $158.1 billion by 2022.
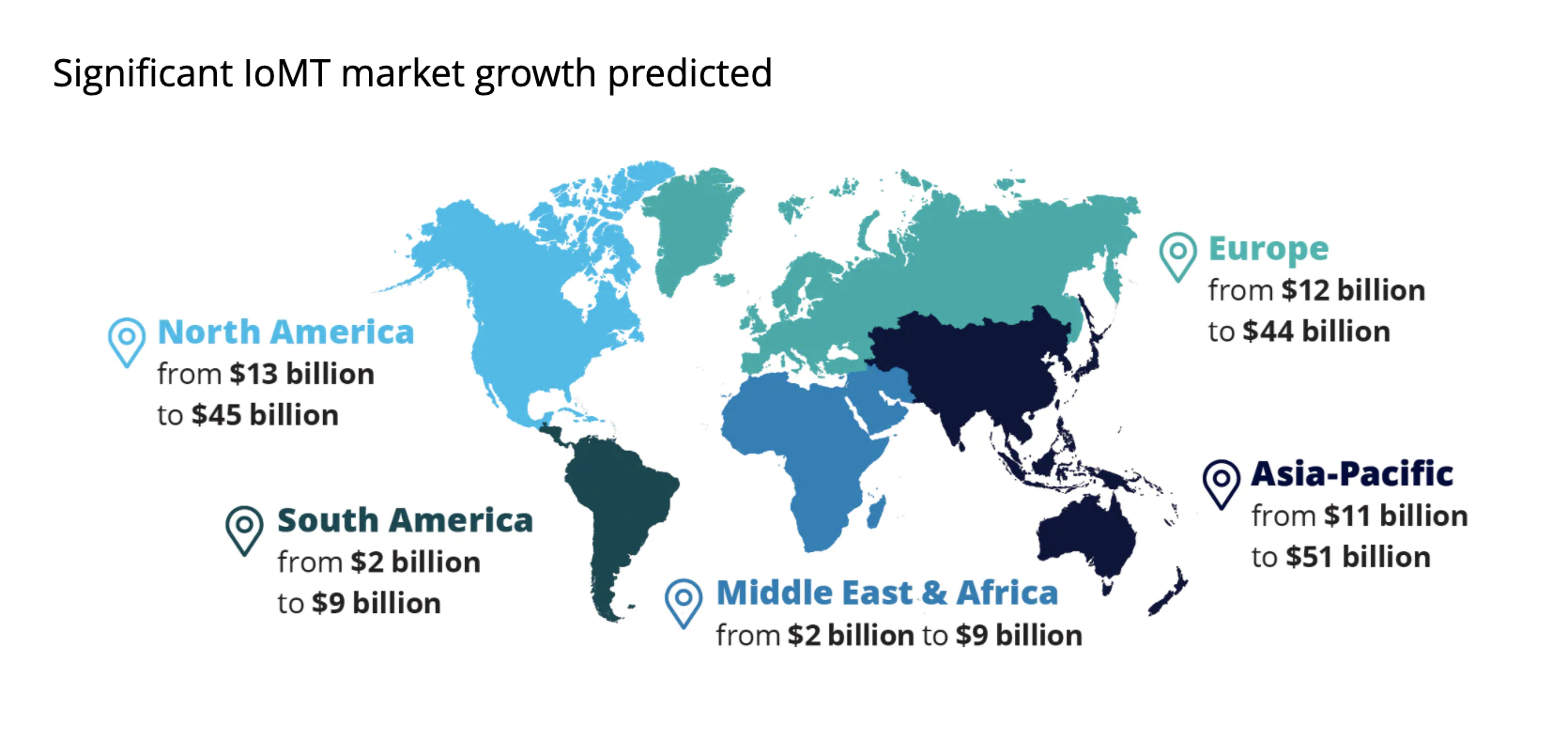
Source: Deloitte
With data being at the heart of healthcare, a seamless data flow between consumers, healthcare providers, insurers and regulators is a must to ensure effective virtual care. But given the variety of vendors, systems, healthcare platforms, and medical devices, data formats can vary, too, leading to data silos and impeding health data exchange.
The pandemic has exposed the urgent need for radically interoperable data that can be easily shared between providers in real time. To achieve this goal, the US Department of Health and Human Services (HHS) finalized two rules in March 2020 with two main objectives — to promote the interoperability principles and to provide patients with better control over their health data.
Deloitte’s survey on the future of virtual health revealed that as much as 94% of industry leaders expected next-gen interoperability solutions to be the industry norm by 2030.
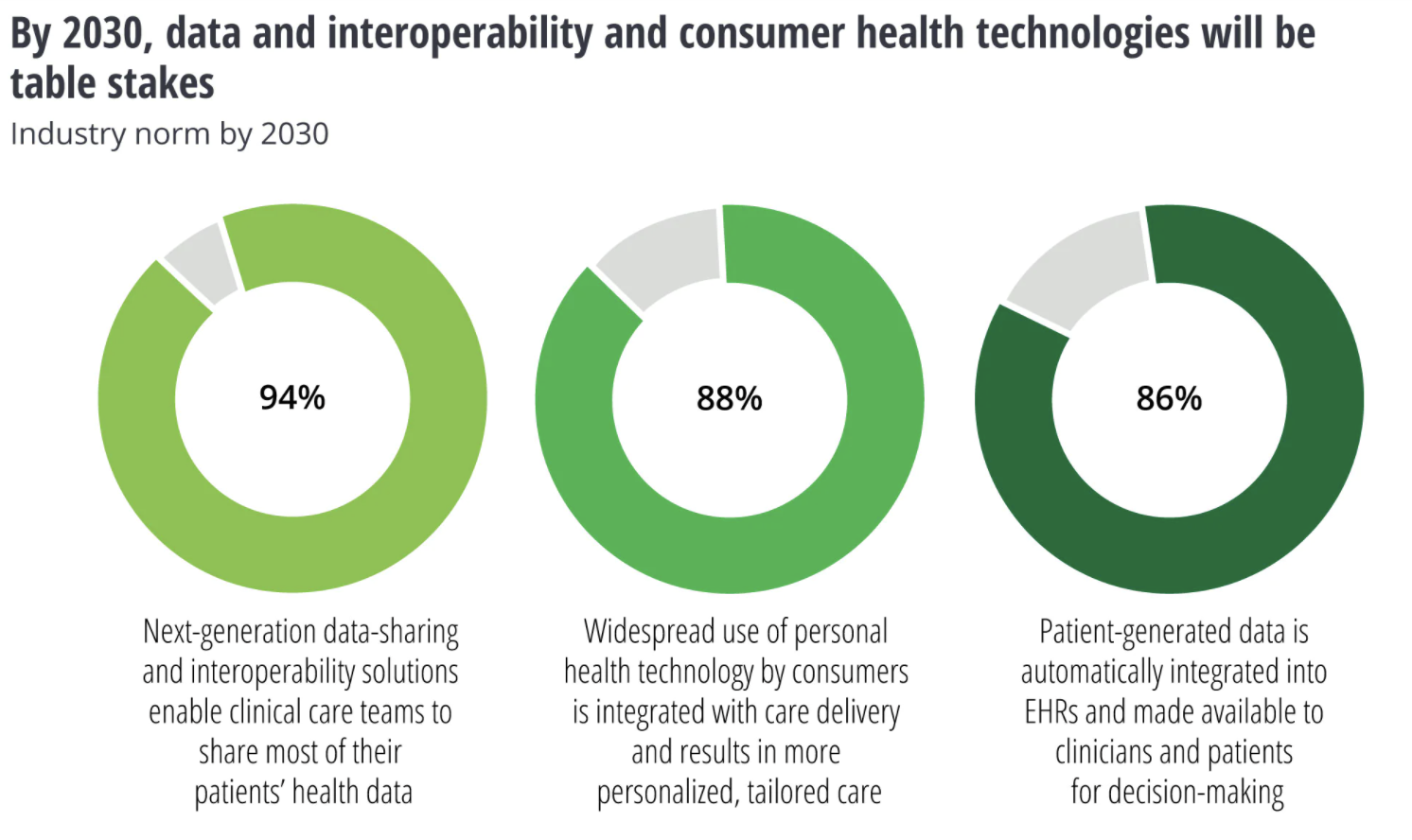
Source: Deloitte
From automating administrative tasks to informing clinical decision-making, artificial intelligence has been making significant strides in the healthcare space. Now as COVID-19 has redefined healthcare needs, the adoption of AI technology has become “a top three thought process for major stakeholders in healthcare”, according to Vince Vickers, KPMG Healthcare Technology Leader.
With the ability to quickly process vast amounts of medical data and uncover hidden patterns, AI can help healthcare and life sciences professionals track the infection spread and accelerate drug discovery. Deep learning, a subset of AI, enables physicians to automate clinical image analysis and identify even the slightest abnormalities, which significantly speeds up clinical workflows and improves diagnostics accuracy.
The rise of telehealth comes with its own set of challenges, one of which is cybersecurity. Healthcare has always been a target for cyberattacks, but as the landscape is being continuously expanded with new technological solutions and connected devices, the attack surface increases, too. Moreover, relaxed regulations around telemedicine services made it easier for patients to access much-needed care but also put data privacy at risk.
Securing the future of virtual healthcare is a shared responsibility and requires the participation of all stakeholders. To ensure patient’s data privacy, healthcare organizations need to transition from consumer-grade video conferencing platforms to HIPAA-compliant healthcare solutions that employ robust security protocols, end-to-end encryption, multi-factor authentication, configuration management, active monitoring, and other technical safeguards.
With the abundance of home medical devices and wearables that transmit critical health data, medical device manufacturers need to implement adequate firmware and hardware-based safety controls to minimize security risks.
In a matter of one year, we have seen virtual care go from extremely rare to a near-default option across a range of care delivery applications. Virtual urgent and non-urgent care, multi-specialty consults and follow-up visits, remote patient monitoring and telepsychiatry services — virtual healthcare is stepping up to close care gaps and improve patient outcomes.
Moving into the post-pandemic future, technology will continue to shape up the healthcare landscape. From wearables to smart medical devices, digital health tools will become more widespread and enhanced with AI capabilities. But to ensure that all pieces of the puzzle work together, a greater focus on data interoperability and security is needed.



