
Did you know that today there are an estimated 2 million different kinds of medical devices on the global market according to WHO? From glucose monitors and fitness bracelets to robotic surgery systems, the medtech industry is continuously growing. By 2030, the annual sales around the globe are expected to reach about $800 billion.
Due to that, one might expect a well-connected healthcare ecosystem with seamless health data exchange between all the parts involved. But the reality tells a different story. About 80% of serious medical errors involve miscommunication between care teams, which is the result of siloed and fragmented systems.
This is why seamless medtech integration is crucial. By consolidating data from various devices and making it easily accessible, integration reduces errors and fosters a more connected and efficient care environment.
Just like a traffic control system orchestrates seamless movement of vehicles to avoid chaos, software integration ensures that all healthcare technology solutions and devices are working together to avoid errors and miscommunications. Below are some of the advantages of this harmony.
For patients, medtech integration means quicker, more accurate care. Real-time data from devices like wearables and monitors helps doctors identify issues earlier, reducing medical errors and improving outcomes. Plus, a person’s medical history is connected at every step making healthcare experiences smoother and less stressful.
For clinicians, integration removes the hassle of manual data entry, freeing up time to focus on what really matters—patients. It also bridges communication gaps between departments, enabling seamless collaboration for sharing test results or coordinating treatment plans.
For healthcare organizations, integration boosts efficiency and cuts costs. By eliminating redundant tests and streamlining workflows, providers can allocate resources where they’re needed most. It’s smarter, faster, and ultimately, better care for everyone.
Just like any software development project, medical device integration requires a strategic and phased approach. By breaking down the process into clear, actionable steps, healthcare organizations can tackle challenges effectively and ensure a seamless rollout.
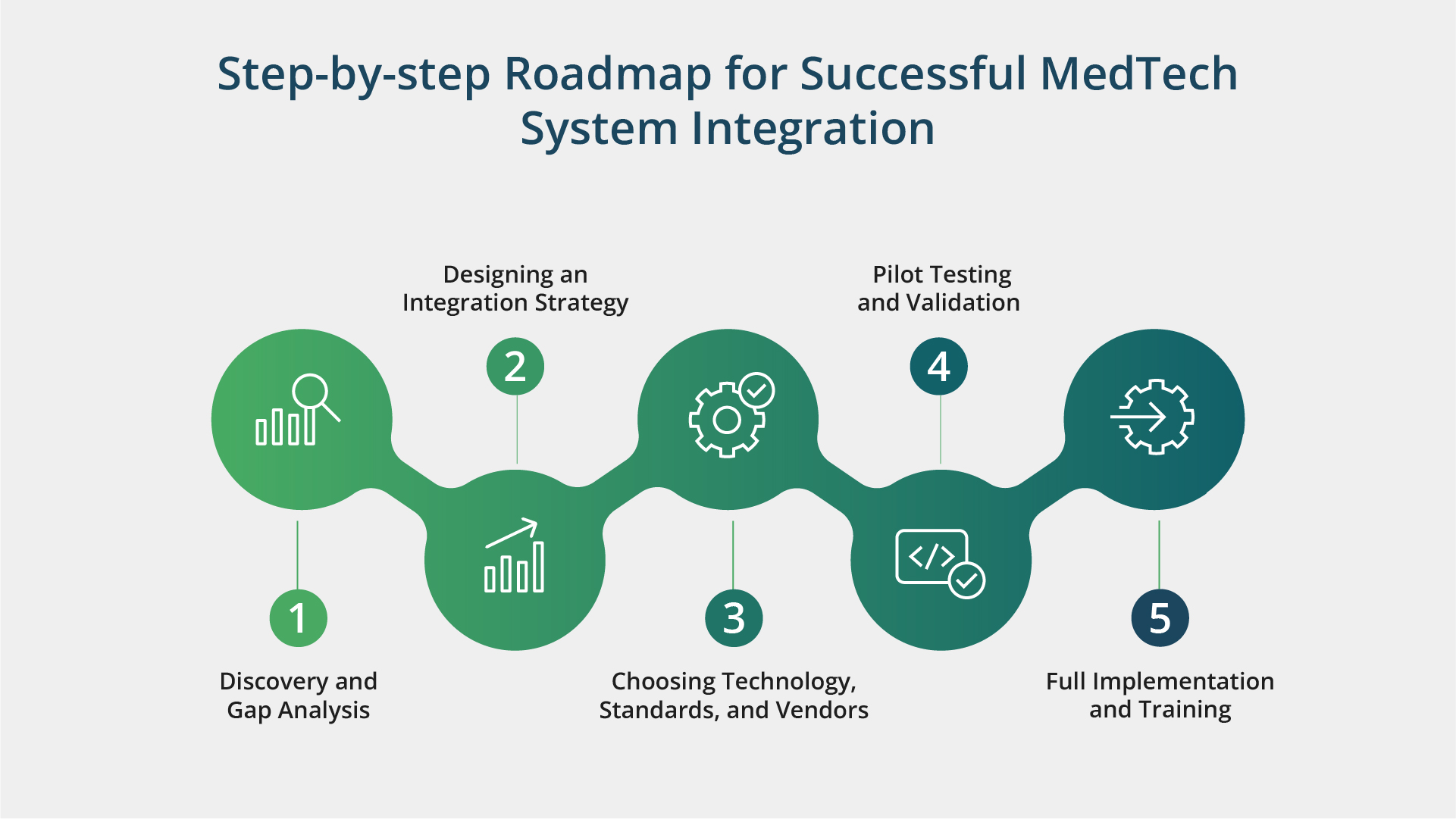
Start by assessing your current technology landscape and identifying what systems, workflows, and data flows are already in place. Find inefficiencies or gaps, such as devices that don’t communicate or manual processes prone to errors. Pinpoint the integration points that will deliver the most value — whether it’s linking an EHR with remote monitoring tools or integrating an AI-powered healthcare solution to support clinical decision-making.
Once you have a clear understanding of your integration needs, the next step is to create a detailed plan. Outline the project’s scope, budget, timelines, and success metrics. Also, don’t forget to build regulatory compliance into your strategy to ensure data security and patient privacy are top priorities.
Selecting the right tools and partners is critical. To guarantee interoperability, look for technologies that are compatible with industry standards such as HL7, FHIR, or DICOM. Evaluate potential vendors for their expertise, scalability, and track record in healthcare integrations. Think long-term — your system should grow alongside your organization’s needs.
To test the integration in a controlled setting, start small by implementing a pilot program in a single clinic or department. Get user feedback, fix workflow or technological problems, and fine-tune the system based on real-time performance.
Once the pilot is successful, increase the scale up to a full rollout. To ensure that clinicians, IT personnel, and administrators feel comfortable utilizing the new technologies, provide them with specialized training. Offer ongoing support to ensure a smooth transition and high adoption rates.
In addition to a clear plan and actionable strategy, successful integration relies on the right partner for a smooth implementation. Check out our comprehensive checklist to guide your decision or reach out to Kanda Software for expert support and tailored solutions.
Integration projects can be technically complex. Look for the providers’ healthcare software development expertise backed by strong engineering teams, a solid portfolio, and relevant case studies. Their depth of technical knowledge will also influence the ability to optimize workflows, troubleshoot effectively, and future-proof integrations.
Clinical data is governed by strict regulations (e.g., HIPAA in the US, GDPR in the EU). Providers must ensure that data is collected, transmitted, and stored according to these regulations. Compliance affects patient safety, organizational liability, and the integrity of clinical workflows. Always look for documented policies, procedures, and certifications (e.g., ISO/IEC 27001, ISO 13485, SOC 2, etc.) that demonstrate regulatory compliance.
Healthcare data is a prime target for cyberattacks. A provider’s ability to secure data both in transit and at rest can help you avoid costly breaches and protect patient privacy. Robust security measures may include encryption protocols, secure authentication mechanisms, network segmentation, and ongoing vulnerability assessments to identify and remediate risks quickly.
Interoperability is the foundation of efficient healthcare delivery. Supporting widely used data standards (e.g., HL7, FHIR, DICOM, IEEE 11073) ensures that devices and systems can communicate seamlessly, reducing manual data entry and minimizing errors. Providers with broad standards support are more flexible and better equipped to integrate with a variety of systems and devices in your ecosystem.
Different integration projects come with different complexities. Hardware integrations often involve unique communication protocols, device drivers, and physical interface requirements. Software integrations, on the other hand, might focus more on APIs, cloud services, or data mappings. A provider’s experience in both realms indicates adaptability and a deeper understanding of end-to-end integration challenges.
Healthcare systems operate around the clock and can’t afford extended downtime. A clear post-integration support model ensures you can get quick help if critical issues arise. Look for providers offering 24/7 or tiered support with documented escalation paths. This level of support is crucial to maintaining device uptime and safeguarding patient care.
Service level agreements (SLAs) outline standards for problem solving and response times. Delays in resolving integration problems in a clinical setting can compromise patient care and increase the risk of noncompliance. SLAs reduce potential downtime and guarantee continuity of care by providing you with contractual assurance that the provider will satisfy specified performance parameters.
Healthcare technology is evolving at breakneck speed, and patient data is growing exponentially. An integration solution that can scale to accommodate new device types and larger data volumes helps avoid costly rework or system overhauls down the road. Ensuring scalability up front allows you to expand services or add new functionalities without disrupting existing workflows.
In today’s rapidly evolving healthcare landscape, medtech system integration is essential for ensuring smooth data interchange, reducing mistakes, and enhancing patient outcomes.
However, successful integration requires a strategic approach, thoughtful planning, and the right technology partner. Kanda Software brings to the table a wealth of experience in developing and integrating value-adding sophisticated health IT systems. Kanda makes sure your systems interact efficiently and securely by integrating advanced interoperability protocols like HL7 and FHIR and adhering to regulations like HIPAA and GDPR. Contact us today to start your integration journey.



